Case StudiesQuiz of the month – April 2023
Take our patient case study quiz specially curated for you by our Faculty Member, Prof. Samer Ellahham.
Prof. Samer Ellahham
First published: April 17, 2023
Case Study: A 65-year-old man with a history of dyslipidemia, type 2 diabetes mellitus and systemic hypertension.
Presentation: | New onset crescendo angina x 5 days culminating Rest pain for the past 2h No history of other vascular events or heart attack, no TIA or stroke Weight: 90 kg Exam: BP 150/85 (slightly elevated), Heart Rate 80 No murmur detected |
Medication: | Valsartan 160 mg daily, Aspirin 81 mg daily, Rosuvastatin 10 mg daily, Metformin 500 mg twice daily |
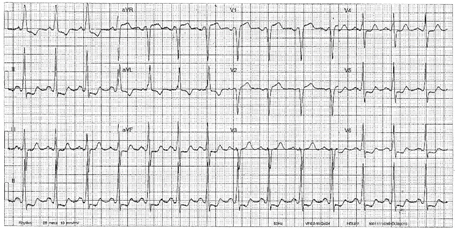
Labs: | BMI 31kg/m2, waist circumference 101.6 cm (40 inches), (-) tobacco (quit last year – 60-pack-year history) Normal CBC, electrolytes Troponin: Elevated Electrocardiogram:1-2 mm horizontal ST depression infero-lateral leads 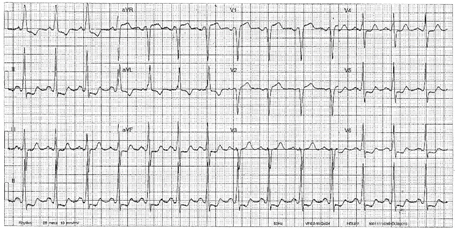
Chest X-ray: Normal |
Lipid panel: | Total cholesterol (TC) 192 mg/dL HDL-C 46 mg/dL Triglycerides 180 mg/dL (non-fasting) LDL-C 110 mg/dL Non-HDL-C 146 mg/ dL |
What are the first impressions about this patient?
Case StudiesCase Study – December 2022
Our patient case study specially curated for you by our Faculty Member, Prof. Samer Ellahham on concerns about statin associated Diabetes Mellitus.
Prof. Samer Ellahham
First published: December 9, 2022
Case Study: RS is a 64-year-old Male having dyslipidemia.
Vital parameters: | BP 144/87 mm Hg Low-density lipoprotein cholesterol (LDL-C) 112 mg/dL High-density lipoprotein cholesterol (HDL-C) of 47 mg/dL Triglycerides 190 mg/dL (-) tobacco, (-) alcohol Body mass index (BMI) 33 kg/m2 |
Medication: | Valsartan 80 mg/d |
Family history: | Father developed type 2 diabetes mellitus (T2DM) and ASCVD at age 58 |
Labs: | Fasting blood glucose 103 mg/dL HbA1C 5.8% Serum Creatinine 1.1 mg/dL Urinary analysis within normal limits |
RS reports that he is reluctant to take statins as they cause diabetes especially with his family history.
Case StudiesQuiz of the month – April 2022
Take our patient case study quiz specially curated for you by our Faculty Member, Prof. Samer Ellaham.
First published: April 7, 2022
Case Study: A 63-year-old male presents with central chest and vague left shoulder pain precipitated by a brisk walk up a steep hill. His pain resolved with rest. He is known to have three vessel coronary artery disease based on two previous cardiac catheterizations. He does more than 40 minutes of cardiovascular exercise at least four days a week, has no history of tobacco or drug use, and does not have diabetes.
Vital Parameters | Blood pressure: 110/65 mm Hg Resting heart rate: 65 Body mass index (BMI): 24 |
Medications | 40 mg of Atorvastatin, daily 81 mg of aspirin, daily |
Investigations | Lipid Profile: High-density lipoprotein (HDL) = 65 mg/dl Low-density lipoprotein (LDL) = 50 mg/dl |
The repeat cardiac catheterization reveals greater than 95% occlusion of his left main coronary, left circumflex, left anterior descending, and posterior descending arteries; and right main coronary artery has approximately 50% stenosis. Based on the diagnosis (high risk of CVD/CHD), he was treated with four-vessel coronary artery bypass grafting surgery, after which he returned to his functional baseline of vigorous exercise without angina. However, as The European Atherosclerosis Society consensus panel recommends, screening for anyone at an intermediate or high risk of CVD/CHD with an Lp(a) goal level of < 50 mg/dl, the cardiologist recommended measurement of Lp(a) which revealed an elevated Lp(a) level of 230 nmol/L, which is in the highest quartile.
Case StudiesQuiz of the month – January 2022
Take our patient case study quiz specially curated for you by our Faculty Member, Prof. Christopher Cannon.
First published: January 10, 2022
Case Study: David is a 63-year-old man with a 20-year history of hypercholesterolemia and 5-year history of prediabetes. When the hypercholesterolemia was diagnosed, his LDL-C was 256 mg/dL. Since then, he has been managed primarily with high-intensity statin treatment (rosuvastatin 40 mg/d), dietary modification (low saturated fat diet), and daily exercise. One year ago, cardiology workup identified evidence of ASCVD (see chart below). At the time, David’s LDL-C was 162 mg/dL on treatment with maximal dose rosuvastatin, so the cardiologist recommended adding ezetimibe 10 mg qd. After 6 months of treatment, David’s LDL-C fell to 134 mg/dL.
Medical History | Hypercholesterolemia, 20 years Prediabetes, 5 years |
Vitals | Heart rate: 72 bpm Blood pressure: 118/74 mmHg Respiration rate: 18 bpm Temp: 98.6 |
Physical examination | Heart: normal sinus rhythm Lungs: clear to auscultation Extremities: no edema Skin: unremarkable Joints: no tendon xanthomas BMI: 23.5 kg/m2 |
Investigations | Today: Random blood glucose: 103 mg/dL A1C: 5.8% [normal <5.7] eGFR: 77 mL/min/1.73m2 Lipid panel: – LDL-C 134 mg/dL – HDL-C 52 mg/dL – Triglycerides 68 mg/dL – Total cholesterol 176 mg/dL One year ago: CT angiogram: high coronary artery calcium, nonocclusive atherosclerosis |
Medications | Rosuvastatin 40 mg qd Ezetimibe 10 mg qd |
Based on his diagnosis of established ASCVD, the cardiologist identified an LDL-C goal <70 mg/dL and added a PCSK9 inhibitor.
It has been 6 months since he started the PCSK9 inhibitor. He returned to the clinic today for a checkup. Workup identifies LDL-C 47 mg/dL. David reports good adherence to therapy and no side effects of treatment with rosuvastatin 40 mg, ezetimibe 10 mg qd, and a PCSK9 inhibitor.