Case StudiesQuiz of the month – April 2023
Take our patient case study quiz specially curated for you by our Faculty Member, Prof. Samer Ellahham.
Prof. Samer Ellahham
First published: April 17, 2023
Case Study: A 65-year-old man with a history of dyslipidemia, type 2 diabetes mellitus and systemic hypertension.
Presentation: | New onset crescendo angina x 5 days culminating Rest pain for the past 2h No history of other vascular events or heart attack, no TIA or stroke Weight: 90 kg Exam: BP 150/85 (slightly elevated), Heart Rate 80 No murmur detected |
Medication: | Valsartan 160 mg daily, Aspirin 81 mg daily, Rosuvastatin 10 mg daily, Metformin 500 mg twice daily |
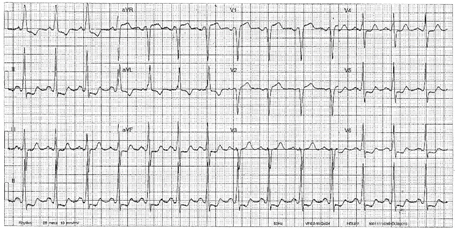
Labs: | BMI 31kg/m2, waist circumference 101.6 cm (40 inches), (-) tobacco (quit last year – 60-pack-year history) Normal CBC, electrolytes Troponin: Elevated Electrocardiogram:1-2 mm horizontal ST depression infero-lateral leads 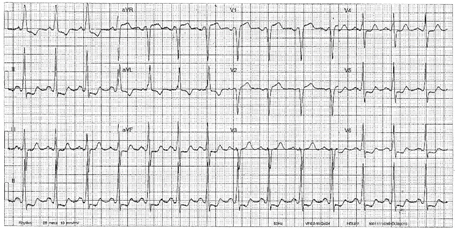
Chest X-ray: Normal |
Lipid panel: | Total cholesterol (TC) 192 mg/dL HDL-C 46 mg/dL Triglycerides 180 mg/dL (non-fasting) LDL-C 110 mg/dL Non-HDL-C 146 mg/ dL |
What are the first impressions about this patient?
Case StudiesCase Study – December 2022
Our patient case study specially curated for you by our Faculty Member, Prof. Samer Ellahham on concerns about statin associated Diabetes Mellitus.
Prof. Samer Ellahham
First published: December 9, 2022
Case Study: RS is a 64-year-old Male having dyslipidemia.
Vital parameters: | BP 144/87 mm Hg Low-density lipoprotein cholesterol (LDL-C) 112 mg/dL High-density lipoprotein cholesterol (HDL-C) of 47 mg/dL Triglycerides 190 mg/dL (-) tobacco, (-) alcohol Body mass index (BMI) 33 kg/m2 |
Medication: | Valsartan 80 mg/d |
Family history: | Father developed type 2 diabetes mellitus (T2DM) and ASCVD at age 58 |
Labs: | Fasting blood glucose 103 mg/dL HbA1C 5.8% Serum Creatinine 1.1 mg/dL Urinary analysis within normal limits |
RS reports that he is reluctant to take statins as they cause diabetes especially with his family history.
Case StudiesQuiz of the month – November 2022
Take our patient case study quiz specially curated for you by our Faculty Member, Prof. Chern-En Chiang.
Prof. Chern-En Chiang
First published: November 8, 2022
Case Study: A 48 y male patient presented with anterior chest pain for 1 hour. He was sent to ER where acute anterior ST-elevation MI was diagnosed. Emergent cardiac catheterization demonstrated a 30-40% stenosis over left main artery, a 100% occlusion over middle portion of left anterior descending artery, 90% stenosis over middle portion of right coronary artery, and a 50% stenosis in the proximal portion of left circumflex artery. Two DES were implanted uneventful: one on LAD and the other on RCA. Echocardiogram revealed an LVEF 52% with mild hypokinesis over LV anterior wall.
Past history: | Type 2 diabetes for 5 years with metformin 1000 mg/d Hypercholesterolemia under rosuvastatin 10 mg/d Denied history of HT No smoking history |
Family history: | Strong family history of premature CVD (His father died of MI at the age of 58. His grandfather died of MI at the age of 65, and his uncle has TVD.) |
Before discharge: | BMI 25 BP 128/76 mmHg, HR 76/min eGFR 76 ml/min, Na 141 meq/L, K 4.1 meq/L HbA1c 7.1% LDL-C 124 mg/dL, HDL-C 42 mg/dL, triglyceride 210 mg/dL, Lp(a) 105 mg/dL |
Discharge medications: | Aspirin 100 mg QD, ticagrelor 90 mg BD, bisoprolol 5 mg QD, metformin 850 mg BD, dapagliflozin 10 mg QD, rosuvastatin 20 mg QD, ezetimibe 10 mg QD |
3-month follow-up clinic: | No symptom BMI 24 BP 120/72 mmHg, HR 66/min eGFR 72 ml/min, Na 144 meq/L, K 4.2 meq/L HbA1c 6.4 % LDL-C 77 mg/dL, HDL-C 48 mg/dL, triglyceride 198 mg/dL, Lp(a) 108 mg/dL |
Case StudiesQuiz of the month – June 2022
Take our patient case study quiz specially curated for you by our Faculty Member, Prof. Chern-En Chiang.
Prof. Chern-En Chiang
First published: June 7, 2022
Case Study: A 67-year-old male comes to the ER with the complaint of excruciating anterior chest pain for 1-hour. The parameters measured in the ER are as follows:
Vital parameters | Blood pressure: 146/78 mm Hg Heart rate: 92/min Respiratory rate: 16/min |
ECG shows ST elevation over V1-V3, suggesting acute anterior MI, and pathological Q waves over leads II, III and aVF. Toponin I was 15.40 ng/mL. Urgent coronary angiograph shows total occlusion over LAD-M, patent left main, patent left circumflex, and 80% stenosis over RCA-M. Left ventriculogram showing moderate hypokinesis over anterior septal area and mild hypokinesis over inferior wall with an EF of 44%. Primary PCI with 2 DES over LAD-M and RCA-M was performed uneventfully.
Past history | Inferior myocardial infarction 4 years with medical treatment HT for more than 10 years with regular treatment Type 2 diabetes for 8 years Denied smoking Obesity with a BMI of 30.5 |
Lab data | Na 134 meq/L, K 4.2 meq/L Cr 1.05 mg/dL, eGFR 73 mL/min (CKD-EPI), UACR 350 mg/g ALT 32 mg/dL HbA1c 8.3% LDL-C 98 mg/dL, HDL-C 28 mg/dL, triglyceride 259 mg/dL Toponin I 15.40 ng/mL, hs-CRP 18.2 mg/dL Lp(a) 83 mg/dL [upper limit of normal Lp(a) = 30 mg/dL] |
Medication history
before admission | Amlodipine 5 mg OD, valsartan 160 mg OD, bisoprolol 5 mg OD Metformin 850 mg BD Aspirin 81 mg OD Atorvastatin 20 mg OD |
Investigation | Acute MI after successful PCI, and this is a second MI (previous inferior MI) Post-MI LV dysfunction (LVEF of 44%) Uncontrolled diabetes (HbA1c 8.3%) Suboptimal control of lipid levels (LDL-C 98 mg/dL) A very high level of Lp(a) (83 mg/dL) |
Case StudiesQuiz of the month – January 2022
Take our patient case study quiz specially curated for you by our Faculty Member, Prof. Christopher Cannon.
First published: January 10, 2022
Case Study: David is a 63-year-old man with a 20-year history of hypercholesterolemia and 5-year history of prediabetes. When the hypercholesterolemia was diagnosed, his LDL-C was 256 mg/dL. Since then, he has been managed primarily with high-intensity statin treatment (rosuvastatin 40 mg/d), dietary modification (low saturated fat diet), and daily exercise. One year ago, cardiology workup identified evidence of ASCVD (see chart below). At the time, David’s LDL-C was 162 mg/dL on treatment with maximal dose rosuvastatin, so the cardiologist recommended adding ezetimibe 10 mg qd. After 6 months of treatment, David’s LDL-C fell to 134 mg/dL.
Medical History | Hypercholesterolemia, 20 years Prediabetes, 5 years |
Vitals | Heart rate: 72 bpm Blood pressure: 118/74 mmHg Respiration rate: 18 bpm Temp: 98.6 |
Physical examination | Heart: normal sinus rhythm Lungs: clear to auscultation Extremities: no edema Skin: unremarkable Joints: no tendon xanthomas BMI: 23.5 kg/m2 |
Investigations | Today: Random blood glucose: 103 mg/dL A1C: 5.8% [normal <5.7] eGFR: 77 mL/min/1.73m2 Lipid panel: – LDL-C 134 mg/dL – HDL-C 52 mg/dL – Triglycerides 68 mg/dL – Total cholesterol 176 mg/dL One year ago: CT angiogram: high coronary artery calcium, nonocclusive atherosclerosis |
Medications | Rosuvastatin 40 mg qd Ezetimibe 10 mg qd |
Based on his diagnosis of established ASCVD, the cardiologist identified an LDL-C goal <70 mg/dL and added a PCSK9 inhibitor.
It has been 6 months since he started the PCSK9 inhibitor. He returned to the clinic today for a checkup. Workup identifies LDL-C 47 mg/dL. David reports good adherence to therapy and no side effects of treatment with rosuvastatin 40 mg, ezetimibe 10 mg qd, and a PCSK9 inhibitor.